What is Cervical Mucus & Why is it Key to Fertility Awareness & Cycle Tracking?
Updated June 11, 2025

Cervical mucus (also called cervical fluid, CM or CF) is the primary sign of fertility and plays an amazing role in our health and fertility. Along with tracking your BBT, tracking your cervical mucus will give you unbelievable insight into not only your fertility, but also your overall health! Ovulation and the menstrual cycle is the fifth vital sign for women.
CM is produced in the cervix, which is the opening to the uterus and is situated between it and the vagina. The cervix has something called cervical crypts, which create the different types of cervical mucus depending on your body's sex hormone levels (most notably estrogen and progesterone). Each has its own purpose in your fertility and health.
Now before we go on, you should know this important rule of thumb: if you ever see cervical mucus through your charting observations prior to confirmed ovulation, you should always consider yourself to be fertile for that day and the three days following.
What is cervical fluid?
Cervical fluid serves two main purposes:
- To sustain and move sperm when you’re fertile
- To protect against infection both when you’re fertile and infertile
Sustains & Moves Sperm
First, it creates a more alkaline (basic) environment in the normally sperm-killing acidic vagina, which allows sperm to survive. It nourishes the sperm and also filters out any that are defective. Cervical mucus becomes more wet and slippery as ovulation approaches and, under the influence of a surge in estrogen, it develops "swimming lanes" that give the sperm a clear path to the ovum (egg) released at ovulation. This cervical fluid gives a smooth, wet, or slippery sensation at the vulva. It may look cloudy or clear, and may be creamy (like lotion) or stretchy like egg-whites - or somewhere in between. Without cervical mucus, the sperm wouldn’t be able to swim fast enough to reach the ovum and would die!
This is why having cervical mucus is so key to conceiving. If you are experiencing little or no cervical fluid, you may have a hormonal imbalance or nutritional deficiency. Many women also experience less optimal cervical mucus after using hormonal birth control and may experience a decrease in cervical fluid with conditions like bacterial vaginosis and yeast infections (and some STIs). Don’t worry, cervical mucus quality and consistency can be improved! (Check out this article.)
Protects Against Infection
Second, cervical fluid protects the uterus and reproductive organs as a whole from infection. After ovulation, progesterone is the dominant hormone. Progesterone causes the cervix to produce a different fluid, which becomes a dense plug that closes the opening of the cervix. This plug is nearly impenetrable to sperm and harmful bacteria. When this cervical plug is in place, you should observe a dry sensation at the vulva. You generally won’t see any cervical mucus when this plug is in place and, if you do, then you may have a hormone imbalance in need of attention.
You may notice some white, dry lines in your underwear (along with a dry sensation at the vulva) even during your infertile phases. Not to worry! This is simply vaginal cell slough and is how the vagina sheds its dead epithelial cells. Vaginal cell slough is not cervical fluid. It’s how the vagina self-cleans and keeps its environment balanced.
Tracking Cervical Mucus - Be Consistent
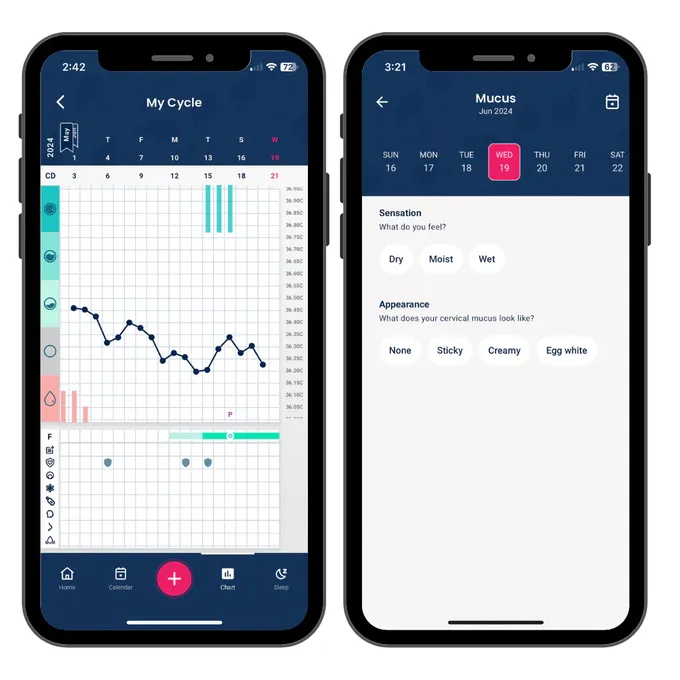
It’s recommended to track cervical mucus by checking every single time you go to the bathroom. You can observe it by wiping before and after going and noting what you feel and see. At the end of the day, you record the most fertile cervical fluid you saw during the day. You can do this either in an app (like Tempdrop's app on /Android) or on a paper chart. Be consistent in how you check, for example by only checking externally by wiping front to back over the vulva. It can take a little time, but developing this habit is key!
You can track your cervical mucus on the Tempdrop app