What is PMDD?
Updated June 11, 2025

Many women experience some level of physical or emotional discomfort during the days leading up to their period, also known as the premenstrual (pre-period) time. Unfortunately, this is something that is joked about (“she’s PMS-ing!”) and expected to be a “normal” part of our cycling experience. This kind of attitude, combined with a lack of education around menstrual health, means that a lot of women aren’t properly diagnosed and end up suffering when they could be supported.
As a medical provider, I want to take some time to explain the difference between PMS and PMDD and why this matters for you and the women in your life you care about.
PMS vs PMDD: What's The Difference?
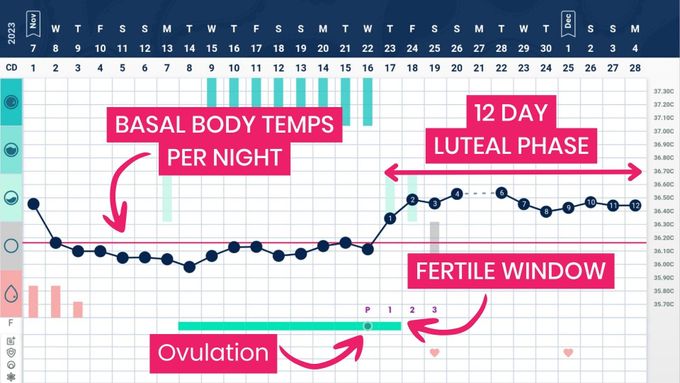
PMS (premenstrual syndrome) and PMDD (premenstrual dysphoric disorder) are both premenstrual disorders. They show up in the mid to late luteal phase (the second half of your cycle after ovulation) and usually ease once your period starts.
Let’s start by looking at PMS.
What Is PMS?
To understand PMDD, I find it helpful to also understand what PMS is first.
PMS is diagnosed when you experience at least one symptom during the luteal phase (Remember this is the time from ovulation to your next period) that disrupts your daily life, but those symptoms clear up soon after your period begins. About 5–8% of women are thought to experience PMS.
PMS symptoms vary and can be physical, emotional, and/or behavioral in nature. The most common reported PMS symptoms include:
Breast tenderness
Abdominal pain
Bloating
Weight gain
Fatigue
Headache
Irritability
Poor concentration
Sleep disturbances
Anxiety
Depression
What Is PMDD?
PMDD (premenstrual dysphoric disorder) is a severe form of PMS with a notable emotional/behavioral component that is associated with significant distress and/or interference with work, school, usual social activities, or relationships with others.
PMDD is diagnosed based on criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5. Here’s what that looks like:
In the majority of menstrual cycles from the last year, at least 5 symptoms must be present in the week before the onset of menses, start to improve within a few days after the onset of your period, and become minimal or absent in the week post-menses
One or more of the following symptoms must be present
Notable affective lability (e.g., mood swings, sadness or tearfulness, or increased sensitivity to rejection).
Notable irritability, or anger, or increased interpersonal conflicts.
Notable depressed mood, feelings of hopelessness, or self-deprecating thoughts.
Notable anxiety, tension, and/or feelings of being ‘keyed up’ or ‘on edge’.
In addition, one (or more) of the following symptoms must be present to reach a total of 5 symptoms:
- Decreased interest in usual activities.
- Subjective difficulty in concentration.
- Lethargy, easy fatigability, or marked lack of energy.
- Marked change in appetite; overeating or specific food cravings.
- Hypersomnia or insomnia.
- A sense of being overwhelmed or out of control.
- Physical symptoms such as breast tenderness or swelling, joint or muscle pain, a sensation of “bloating” or weight gain.
How to Get a PMDD Diagnosis (and necessary support)
The best way to figure out if you have PMDD? Start tracking your cycle and your symptoms.
Keeping a record of when in your cycle your symptoms show up, what they are, and how severe they feel gives your healthcare provider the information they need for an accurate diagnosis.
Without cycle tracking, it’s much harder to tell what’s happening — and you deserve clear answers.
How To Start Tracking Your Cycle?
I recommend and teach the symptothermal method for cycle tracking along with Tempdrop.
Tempdrop makes it easier to confirm ovulation by tracking your basal body temperature and cervical fluid — two key signs that help map out your cycle clearly.
What Happens After a Diagnosis?
Once you’ve gathered your data and received a diagnosis, the next step is finding a healthcare provider who can offer a holistic treatment plan.
This could include:
- Education about PMS or PMDD
- Diet and lifestyle support
- Herbal or supplement options
- Alternative therapies
- Medication, if needed
The goal is empowerment — giving you tools to support your body naturally, not just mask symptoms.
Remember: sharing this information with the women in your life can make a huge difference. Every woman deserves to feel heard and supported.